Appendicitis
Definition of Appendicitis
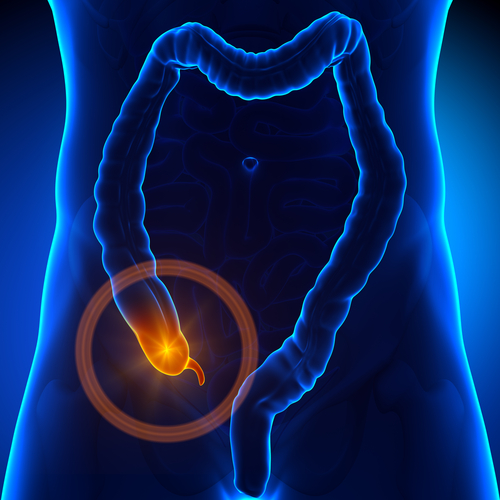 Inflammation of the Appendix, a three and a half inch long tube extending from the Large Intestine, is called Appendicitis. It is also called Epityphlitis and is a surgical emergency.
Inflammation of the Appendix, a three and a half inch long tube extending from the Large Intestine, is called Appendicitis. It is also called Epityphlitis and is a surgical emergency.
First described by Reginald Fitz in 1886, today Appendicitis is the most common cause of severe Acute Abdominal Pain. Case of Appendicitis requires the removal of Inflamed Appendix through procedures such as Laparotomy or Laparoscopy.
The functions of Appendix are still unclear but we can live without it, without any consequences. Untreated Inflamed Appendix eventually burst or perforates causing spilling of infectious material into the abdominal Cavity. This phenomenon leads to Peritonitis. This condition involves the inflammation of the lining of Abdominal Cavity called Peritoneum. Pus filled Abscess also forms outside the inflamed Appendix. Scar tissues of Abscess then separate the Appendix from rest of Abdomen.
Cause of Appendicitis
Blockage of Appendix causes Appendicitis. This blockage can be due to Infection, because Appendix swells in response to any infection of body. Based on the experimental evidence Acute Appendicitis is caused by Primary Obstruction of Appendix Lumen (inside space of a tubular structure). This obstruction causes Appendix to fill up with Mucus as a result of which it swells up. Increasing pressure within the Lumen of Appendix results in two Processes i.e.
-
Thrombosis and Occlusion (blockage due to blood clot) of small vessels
-
Stasis of Lymphatic Flow
In rare cases there is a chance of Spontaneous recovery. If it progresses, Appendix becomes
-
Ischemic (restriction in blood supply to tissues) and
-
Necrotic (cell injury)
Bacteria try to leak through dying walls of Appendix resulting in Pus formation within and around Appendix. This forming of Pus is called Suppuration. The end result of all this is Appendiceal Rupture also called Burst Appendix. Appendiceal Rupture is what leads to Peritonitis that in turn leads to Septicemia (whole body fatal Inflammation) and eventually Death.
Causative agents for Appendicitis are as follows.
-
Foreign bodies
-
Trauma
-
Intestinal worms
-
Lymphadenitis
-
Calcified Fecal Deposit known as Appendicoliths or Fecaliths
Appendiceal Fecalith is associated with Complicated Appendicitis. Fecal Stasis and Fecal Arrest also plays a role in Appendicitis. Acute Appendicitis is an antecedent to following cancers.
-
Colon Cancer
-
Rectum Cancer
Eating Low fiber diet is involved in pathogenesis of Appendicitis. Dietary fibers reduce transit time for Right side of Fecal Reservoir.
Signs and Symptoms of Appendicitis
Common symptoms for Appendicitis are as follows.
-
Dull pain near Navel or Upper or Lower Abdomen, which becomes sharp as it travels to the Lower Right Abdomen. Usually it is the first sign but only occurs in half of the cases.
-
Appetite Loss
-
Nausea and Vomiting
-
Swelling of Abdomen
-
Constipation with Gas
-
Inability to pass Gas
-
Painful Urination
-
Sense of relief after passing Stool
Classic presentation for Acute Appendicitis is
-
Firstly Pain
-
Secondly Vomiting
-
Lastly Fever
Innervation of Appendix enters Spinal Cord at the same level of Umbilicus (Belly Button). Because of this reason, pain starts Stomach-high. As the appendix becomes more swollen with time and irritates the adjoining Abdominal Wall, the pain tends to move into the lower right Abdomen in several hours. Signs of it include:
-
Palpation- sensitivity to gentle pressure on Abdominal Wall.
-
Rebound Tenderness- severe pain on sudden pressure release in Lower Abdomen.
In case of Retrocecal Appendix pressure on right lower abdomen fails to cause tenderness. This is because Cecum is filled with Gas protecting the Inflamed Appendix from pressure. If Appendix lies within Pelvis then Abdominal Rigidness is entirely absent. In these cases Rectal Examination points out tenderness in Rectovesical Pouch. Coughing causes point tenderness in Rectovesical Pouch, the point known as McBurney’s Point.
Risk Factors for Appendicitis
Risk factors for Appendicitis are as follows.
-
Age:
One of the risk factors for Appendiceal perforations is Age. It can occur in all age groups but is common in between ages of 11 and 20.
-
Gender Difference:
Males have higher rate of Perforated Appendicitis than Females. The male to female ratio is (1.4: 1). A male child suffering with Cystic Fibrosis has high risk for developing Appendicitis.
-
Races:
The risk factor for Appendicitis is most common in Whites and Hispanics than African Americans and Asians.
-
Seasonal Variation:
Risk for appendicitis is increased during the winter months between October and May.
-
Prior Antibiotic Administration:
Prior treatment with Antibiotics is also an independent risk factor for Appendicitis.
-
Renal Disease:
In patients with end stage Renal Disease risk factors include the following.
-
Atrial Fibrillation
-
Severe Liver Disease
-
Diabetes Mellitus
-
Hemodialysis
-
Severity of Inflammation:
Increased CRP (C – reactive protein) can be a serious pathological severity for Appendicitis.
-
Other risk factors:
Some of the other factors that contribute to Appendicitis are as follows.
-
Age of children
-
Delay in Surgical intervention
-
Family anamnesis
-
Late recognition of symptoms of Appendicitis
-
Appendicolith:
Recurrent Appendicitis has a rate of 72% in association with presence of Appendicolith. This rate was 26% in those having no Appendicolith.
Diagnosis of Appendicitis
Diagnosis of Appendicitis is based on patient’s History (symptoms) and physical examination backed up by increase in Neutrophil White Blood Cells. Histories are divided into two categories i.e.
-
Typical history includes pain in the abdomen near Umbilicus region for several hours accompanied with nausea and vomiting. The pain then settles in Lower Right Abdomen where it causes tenderness.
-
Atypical history includes the pain in Lower Right Abdomen initially that requires Imaging with Ultrasound or CT scan for diagnosis.
Physical diagnosis of Appendicitis includes following signs:
-
Aure-Rozanova Sign– pain on palpation with finger in right Petit Triangle.
-
Bartomier-Michelson’s Sign– pain on palpation at right Iliac Region when patient lays on his/her left side.
-
Dunphy’s Sign– pain due to coughing in right upper region.
-
Massouh Sign is a firm swish of examiner’s Middle and Index finger from
Xiphoid Process of Sternum to first left and then right Iliac Fossa. Positive sign for it is the grimace of patient upon right sided sweep. It is due to the fact that Appendicitis causes irritation of well innervated Peritoneum.
-
Obturator Sign includes the contact of Appendix with Obturator Internus. Flexion and internal rotation of Hips causes Muscle Spasm. This is known as Obturator Sign.
-
Psoas Sign is also known as Obraztsova Sign. It causes pain in the right lower region upon two conditions while supine i.e.
-
Passive Extension of patient’s right hip
-
Passive Flexion of patient’s right hip
-
-
Rovsing’s Sign is continuous palpation on Left Iliac Fossa causing pain in Right Iliac Fossa. This is due to pushing of bowel contents towards Ileocaecal Valve which increases pressure around Appendix.
Beside Physical examination some tests are also some test performed for Appendicitis. These tests are as follows.
-
Urinalysis is a test for determining pregnancy status for an Ectopic Pregnancy. It also rules out the Urinary Tract Infection and Kidney Stone.
-
Pelvic Exams is taken to make sure that women don’t have Reproductive problems and also ruling out any Pelvic Infections.
-
Imaging for Appendicitis includes the following.
-
Ultrasound
-
X rays
-
CT Scan
-
Ultrasound is preferred upon X-ray confirming diagnosis with Children. In adults and adolescents CT scan is preferred upon Ultrasound.
Prevention from Appendicitis
Chances of Appendicitis are much lower in people who use High Fiber Diet. The exact reason of it is still unknown, but one possible reason for it is that Fibers make our Stool softer. This reduces the chance of stool getting stuck in Appendix. Foods high in fiber are as follows.
-
Wholegrain
-
Cereals
-
Rice
-
Root Vegetables like Carrot
-
Fruits
Treatment of Appendicitis
Acute Appendicitis is treated with surgery whereas in uncomplicated cases antibiotic can prove useful and safe. The treatment of Appendicitis includes the following.
-
In rare cases Antibiotics and Liquid Diet may help to recover without surgery.
-
Based on the case the surgical removal of Appendicitis is performed. The procedure is called Appendicectomy. There are generally two type of surgery i.e.
-
Laparotomy is the typical surgery for Appendicitis. The procedure includes a single large incision of 2 to 3 inches in lower right region of Abdomen. This surgery is also used to examine structures inside Abdominal Cavity and is known as Exploratory Laparotomy. The time for this surgery is no more than an Hour.
-
Laparoscopic Surgery is a newer procedure for the removal of Appendix. This surgery involves making three to four incisions of 0.25 to 0.5 inches and inserting a surgical tool called Laparoscope in one of the incisions. The other two incisions are for specific removal of Appendix using surgical tools. Recovery time after this surgery is shorter.
-
Open surgery is performed right away if the patient have a ruptured Abscess or Appendix.
